Hormone Replacement Therapy for Women: Your Options Explained.
Clearing the air and debunking common myths
Neuro Athletics is a 2 x weekly newsletter that breaks down the medical and scientific practises that you need to perform at your peak. Subscribers include professional athletes, athletic trainers, coaches and casual fans. So if you are not already a subscriber, sign up and join 67,000+ others who receive it directly in their inbox each week — it’s free.
Story at a Glance:
Menopausal Symptoms and HRT: HRT effectively alleviates vasomotor symptoms, bone density loss, muscle strength decline, mood changes, and reduced libido caused by menopause.
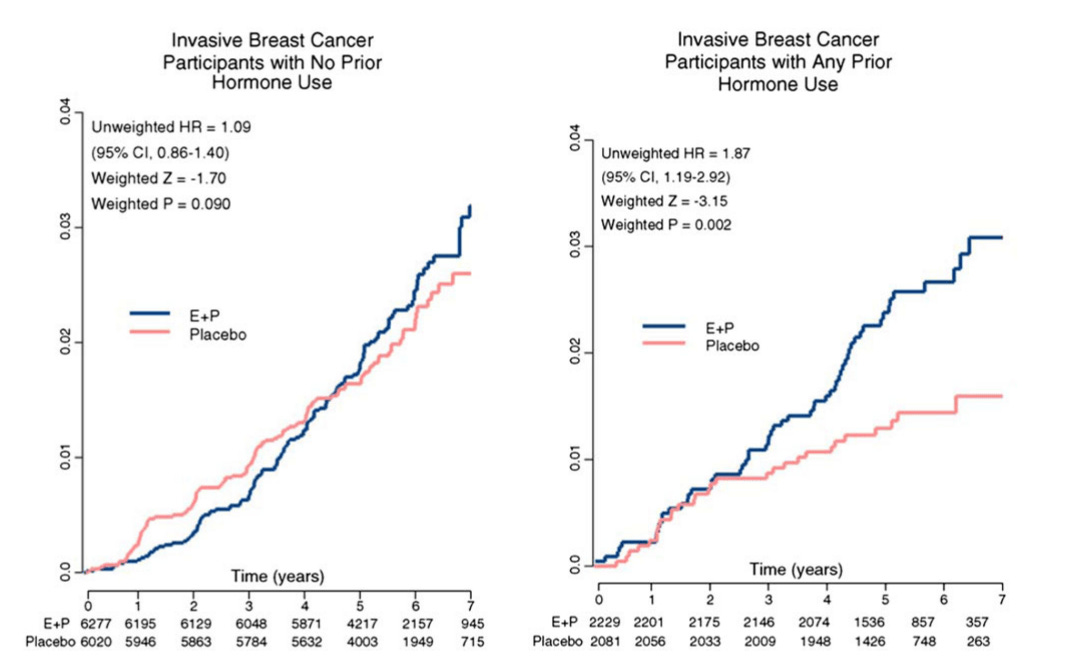
Women's Health Initiative (WHI): The WHI study initially linked HRT to increased breast cancer risk and no cardiovascular benefits, leading to a decline in HRT use. However, flaws in the study design and subsequent analyses revealed overblown risks.
Current Consensus: HRT should be started within the first 10 years of menopause for maximum benefits. The debate continues on long-term use and its associated risks.
Breast Cancer Risk: Recent studies indicate that bioidentical hormones do not increase breast cancer risk, challenging earlier WHI findings.
Read the full article to understand the detailed benefits and risks of HRT.
Today’s Newsletter Is Brought To You By Eight Sleep!
I’ve been using an Eight Sleep mattress for several years now, and it’s one of the best products I’ve ever purchased.
Their thermo-regulation technology — the bed gets colder or warmer throughout the night depending on individualized health metrics — helps me fall asleep faster, get higher-quality sleep, and wake up feeling energized.
Use code NEURO to get $200 off Pod 4 and $350 off Pod 4 Ultra.
Neuro Athletes,
Recently, I uploaded a reel that sparked significant discussion due to Dr. Galanis's statements about HRT. Let me be clear: the benefits of hormone replacement therapy, especially with bioidentical hormones, are strongly supported by current scientific evidence.
It's crucial to distinguish outdated myths from contemporary findings. Advances in medical research and a deeper understanding of hormone biology highlight HRT's benefits for muscle mass, bone health, and cognitive function.
This article will explore HRT options, debunk myths from the Women's Health Initiative, and present the scientific evidence supporting HRT, particularly regarding Alzheimer's disease.
A Brief Refresher on Context
When women go through menopause, levels of the sex hormones estrogen and progesterone plummet, causing vasomotor symptoms (e.g., hot flashes and night sweats) classically associated with this period of a woman’s life. These hormonal changes also result in losses in bone mineral density and muscle strength, changes in mood, decline in libido and sexual function, and various other effects impacting quality of life and physical health. Hormone therapy is intended to attenuate these undesirable symptoms of menopause by providing exogenous estrogen (with or without progesterone) to supplement the body’s low levels.
Observational studies in the 1980s and 90s indicated that HRT might also reduce the risk of cardiovascular disease (CVD) and cognitive decline, motivating Dr. Manson and her fellow researchers to begin the Women’s Health Initiative. This included two randomized clinical trials designed to investigate the efficacy of HRT for chronic disease prevention. However, when the WHI’s results were first published in 2002, the investigators reported no reduction in heart disease among those on HRT, but slightly increased incidence of breast cancer. The media jumped on these findings, causing the use of HRT to plunge by 70-80%.
Since then, many have pointed out that the risks were very overblown. Dr. Manson herself expressed that these results should not be extrapolated to the point of denying HRT to women in early menopause for symptom relief. The debate continues over the magnitude of risks and benefits – and over exactly who should be on HRT and for how long.
On What Do We All Agree (and Disagree)?
HRT is unquestionably the single most effective treatment for easing the symptoms of menopause. Despite the WHI’s reports and subsequent alarmist media coverage, no one disputes HRT’s efficacy in relieving menopausal symptoms and thereby improving quality of life. The debate lies in whether this relief comes at the cost of raising the risk of certain chronic diseases, particularly breast cancer, dementia, and cardiovascular disease.
A point of broad consensus in the medical community is that HRT should only be initiated within the first 10 years of the onset of menopause. Starting hormone therapy more than a decade after menopausal onset means experiencing a prolonged period of estrogen deprivation, which likely diminishes any potential benefits of HRT and may increase any potential risks. For instance, a 2004 meta-analysis of randomized trials reported that women enrolled in hormone therapy trials before age 60 were at significantly reduced all-cause mortality risk relative to placebo (OR: 0.61, 95% CI: 0.39-0.95), but this apparent benefit was absent in women enrolled over the age of 60 (OR: 1.03, 95% CI: 0.90-1.18). The risk of dementia on HRT may also be reduced in those who start treatment during early menopause but may increase in those who begin treatment late. However, this concern only applies to initiating HRT more than 10 years after menopausal onset, which should not be confused with continuing HRT beyond 10 years after menopausal onset.
Whether or not to continue HRT post-menopause is another point of debate. Some believe that hormone therapy comes with an increased risk of disease and is only warranted when menopause symptoms are severe enough to justify the increased risk. These individuals advocate against continuing HRT after menopausal symptoms have subsided, as any other possible benefits are insufficient to offset the risks. Others, myself included, maintain that hormone therapy has substantial positive impacts beyond menopausal symptom relief and that the alleged risks associated with HRT are not supported by evidence, lack clinical significance, or otherwise fail to outweigh the benefits to health and quality of life.
In other words, the decisions to initiate HRT or continue post-menopause boil down to a risk-benefit analysis, and the best choice may vary across individuals based on factors such as menopausal symptom severity, family history, and personal preferences. While I can’t offer a generic, one-size-fits-all answer, I can share what we currently know about the benefits and risks of HRT so that you can make informed decisions for yourself or your patients.
Muscle Mass and HRT
As women age, muscle mass tends to decline, a condition known as sarcopenia. Estrogen plays a critical role in maintaining muscle strength and mass. Studies have shown that estrogen therapy can help mitigate muscle loss in postmenopausal women. Estrogen receptors in muscle cells promote muscle protein synthesis, enhancing muscle strength and function. Thus, HRT can be a valuable tool in preserving muscle health as women age.
Debunking the Women's Health Initiative Myth
The Women's Health Initiative (WHI) study in the late 1990s and early 2000s significantly impacted the perception of HRT. The study suggested an increased risk of breast cancer, heart disease, and strokes among women on HRT, causing widespread fear and a decline in HRT use. However, critical flaws in the study design have since been identified.
The WHI study predominantly involved older women, many years past menopause, and used synthetic hormones, such as conjugated equine estrogens (CEE) and medroxyprogesterone acetate (MPA), which are not bioidentical hormones. Subsequent analyses and studies using bioidentical hormones have shown that HRT, when initiated at the onset of menopause, does not increase breast cancer risk and may even offer protective benefits against cardiovascular disease and cognitive decline.
Get 20% Off My Supplements
One of the biggest benefits of whey protein is its ability to combat age-related muscle mass and strength loss. Starting around the age of 40, individuals can lose approximately 3-5% of their muscle mass per decade, which can significantly impact strength and mobility.
By supplementing with whey protein, you can support muscle maintenance and growth, helping to preserve strength and function as you age.
The best part?
Momentous has by far the most rigorous commitment to quality, demonstrated by expert partnerships and strict third-party testing, making their products a reliable choice upheld by top athletes.
Code: NEURO for 20% off
Bone Health
Osteoporosis, a condition characterized by weakened bones, is a significant concern for postmenopausal women. Estrogen deficiency accelerates bone loss, increasing the risk of fractures. Estrogen therapy has been proven to maintain bone density and reduce fracture risk. Estrogen receptors on bone cells play a crucial role in bone remodeling, promoting bone formation and reducing bone resorption. Thus, HRT is a vital strategy in preventing osteoporosis and ensuring bone health.
Alzheimer's Disease and Cognitive Function
Emerging research highlights the potential cognitive benefits of HRT. Estrogen positively influences brain function by modulating neurotransmitter systems, promoting synaptic plasticity, and enhancing cerebral blood flow. Studies suggest that estrogen therapy may reduce the risk of Alzheimer's disease when started early in menopause. Estrogen receptors are widely distributed in brain regions associated with memory and cognition, such as the hippocampus. By maintaining estrogen levels, HRT helps preserve cognitive function and may delay the onset of Alzheimer's disease.
Estrogen Receptors and Breast Cancer Risk
One of the significant concerns regarding HRT is the risk of breast cancer. However, recent evidence indicates that bioidentical estrogen, especially when combined with natural progesterone, does not increase breast cancer risk. Estrogen receptors in breast tissue respond differently to synthetic hormones compared to bioidentical hormones. Bioidentical hormones mimic the body's natural hormones, reducing the likelihood of adverse effects. Therefore, the risk of breast cancer with HRT, particularly with bioidentical hormones, is minimal.
Types of HRT and Administration Methods
There are various forms of HRT, including:
Oral Pills: Convenient but may increase the risk of blood clots.
Transdermal Patches: Deliver hormones through the skin, reducing the risk of blood clots.
Gels and Creams: Applied to the skin, offering flexibility in dosage.
Vaginal Rings: Provide localized estrogen, helpful for vaginal symptoms.
Pellets: Implanted under the skin, releasing hormones over time.
Bioidentical hormones, which are chemically identical to those produced by the body, are preferred for their safety profile and effectiveness.
Why the Controversy?
The controversy surrounding HRT stems from several factors:
Misinterpretation of the WHI Study: The WHI study's flawed design and subsequent media coverage led to widespread fear and misunderstanding about the risks of HRT.
Historical Use of Synthetic Hormones: Earlier forms of HRT used synthetic hormones, which are not bioidentical and have different safety profiles. The adverse effects seen with these synthetic hormones contributed to the negative perception of HRT.
Lack of Education: Many healthcare providers have not kept up with the latest research on HRT, leading to outdated recommendations and reluctance to prescribe HRT.
Media Sensationalism: Headlines often focus on potential risks without providing context or discussing the absolute risk, leading to public fear and confusion.
Variability in Individual Response: Women respond differently to HRT, and without personalized approaches, some may experience adverse effects, fueling controversy.
Personalized HRT
HRT should be tailored to individual needs, considering factors such as age, health status, and risk factors. Regular monitoring and adjustments are essential to optimize the benefits and minimize potential risks. Collaboration between patients and healthcare providers is crucial to ensure the best outcomes.
What are your thoughts on this?
Let me know in the comments below.
Stay Healthy,
Louisa x








I’ve been on bioidentical hormone therapy cream for over 11 years. I tried tapering down the dosage with my doctor a couple of months ago and I could tell a negative difference in about 2-3 weeks. I went back up to my original dosage and feel back to normal again. Hormone therapy has been a life saver for me.
I was told by my doctor that my propensity for developing blood clots would be increased if I started using hormones. It’s a genetic thing, prothrombin and factor V Leiden. So, it’s off the table.